I. The Unspoken Side of Recovery
Before a patient goes to surgery, they’re taught what to do and what to expect. They learn which medications to take or hold, when to stop eating, and which soaps or wipes to use the night before. They’re briefed on what the surgeon will do and how long the recovery might take.
But what patients rarely hear about is the emotional work that begins once the surgery is over. The days that follow can bring fear, frustration, and uncertainty – feelings that no discharge paper can fully prepare them for. Closing the incision is only part of the job; the real healing is helping patients adjust, understand, and regain confidence afterward.
As nurses, we see how emotions quietly shape every step of recovery. A calm explanation can lower anxiety. A few extra minutes of reassurance can turn confusion into trust. Emotional healing may not be charted in the record, but it influences every outcome just the same.
II. The Emotional Shock After Surgery
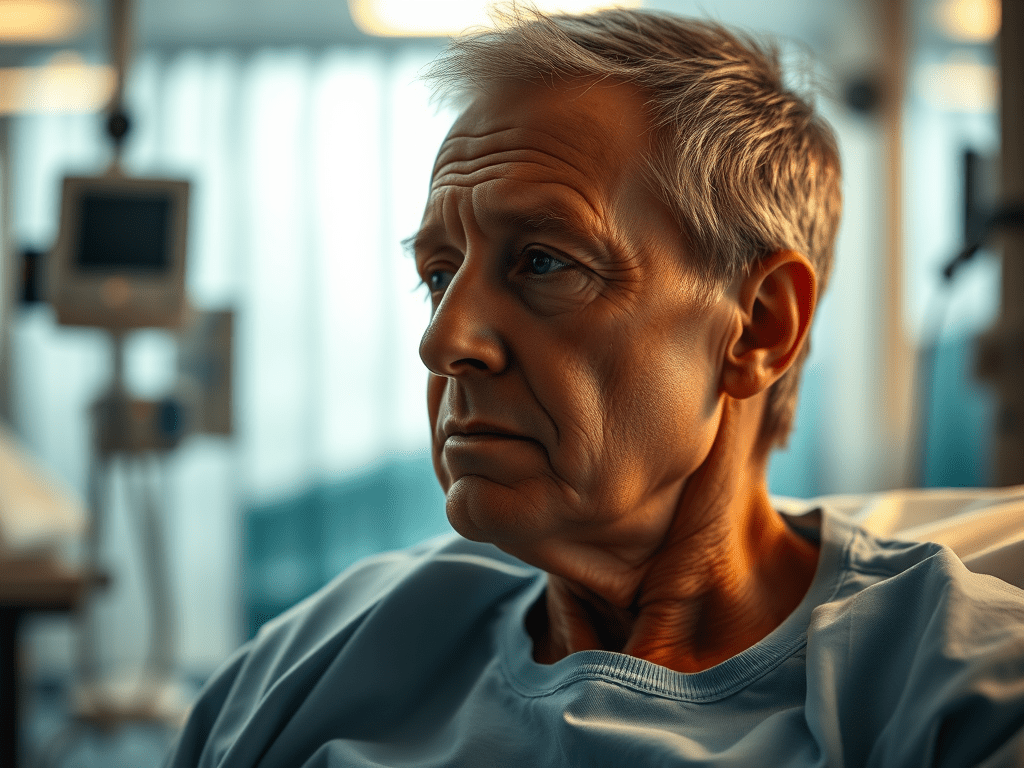
Many patients expect that after surgery, they’ll have some swelling, pain, or limited movements. What they don’t expect is the emotional rollercoaster that follows. Waking up after surgery, a patient can experience a wide range of emotions – many of which take them by surprise.
Fear and Vulnerability
There’s a sudden loss of control. Simple actions like sitting up, walking, or reaching for a cup of water now require help. Patients find themselves depending on strangers – nurses and aides – to provide medications, assist with hygiene, or help them to the bathroom. That dependency can feel unsettling, especially for those use to managing on their own.
Frustration
Frustration sets in when recovery doesn’t match the expectations they had before surgery. Small setbacks – like pain during movement or slower progress – can feel like personal failure, even when it’s completely normal.
Isolation
Many patients also describe feeling isolated. The hospital routine moves quickly, with staff coming and going. Faces change often, and visits from family or friends may be limited. Even surrounded by care, it’s easy for patients to feel unseen or alone.
Each of these emotions can trigger the body’s stress response, even as the physical healing process begins. The body may be resting, but the mind is still trying to make sense of what happened – and that invisible recovery is just as important to recognize.
III. What’s the Body Doing & The Nursing Role
In a previous post, I talked about why a patient’s throat may hurt after surgery and how that can be completely normal. What I didn’t mention was how anxiety-inducing those unfamiliar sensations can be when a patient doesn’t know they’re normal. A sore throat is just one small example – there are many physical symptoms after surgery that can spark unnecessary worry simply because the patient doesn’t understand them.
That anxiety alone can create new physical symptoms. I once cared for a patient recovering from abdominal surgery who believed something was terribly wrong. He hadn’t said anything, but when I checked on him, he was sweating and restless – his blood pressure and heart rate were both elevated. Physically, nothing was wrong; it was anxiety showing up through his body. Moments like that remind me how deeply the mind and body communicate during recovery.
My role as a nurse is to care for both sides – the physical and the emotional. I’ve learned that even small interactions can shape a patient’s sense of safety. I never rush or hover over them with half of my attention. Patients who feel like they’re a bother or unimportant often hold back their questions and fears, which can delay healing. Facing the patient, listening fully, and answering calmly matters just as much as any medication I give.
To help ease that loss of control, I take time to explain what’s coming next during my shift — when medications are due, when vital signs will be checked, and what goals we’ll work toward, like walking or sitting up. These conversations give anxious patients something steady to hold onto. One patient once told me, “Thank you. I felt so scared, but I didn’t want to say anything because I thought it was stupid to feel that way.” That moment has always stayed with me.
It’s a reminder of why I approach recovery the way I do — the guest in my care should never be afraid to speak if I can do something to ease that fear.
IV. The Patient’s Inner Journey
One of the first things a patient learns after surgery is that healing comes with temporary limits. What once felt simple—walking to the bathroom, lifting a cup, or turning over in bed—can suddenly feel like climbing a mountain. It’s easy to feel discouraged, but recovery isn’t about how fast you return to normal; it’s about finding progress in the small victories.
Sitting up for the first time, keeping food down, or taking a few steady steps are all milestones worth celebrating. These moments might seem minor, but they’re signs that the body is doing exactly what it should. When patients focus only on what they can’t do, frustration grows and motivation fades. That’s why it’s so important to know when to rest and when to push forward.
Healing isn’t a race—it’s a dialogue between strength and patience. If your body needs more time, it’s not failing; it’s protecting. Each day it allows you to do a little more, it’s proving that repair is underway, even if you can’t see it yet.
V. Emotional Healing at Home: What Families Should Know
When your loved one comes home from surgery, it helps to know what to expect. Recovery isn’t only physical; it’s emotional too. The moods that surface after surgery can be unpredictable—ranging from sadness to irritability, or from quiet withdrawal to bursts of frustration. Please don’t take these shifts personally. They’re often the mind’s way of catching up to what the body has been through.
Encourage rest without smothering. Patients who feel constantly monitored may also feel a loss of control, which can make them anxious or discouraged. Gentle guidance and space to breathe help them regain a sense of independence.
Celebrate the small milestones. When your loved one walks to the bathroom without help, eats without nausea, or moves around with less pain, acknowledge it out loud. These moments give a sense of progress and remind them that healing is happening.
When you communicate, try using open-ended questions instead of quick check-ins. Ask things like, “How are you feeling today?” or “What feels different from yesterday?” This not only invites honest reflection but also gives you a better understanding of how recovery is going—emotionally and physically.
Nursing Note: Family calmness often become’s the patient’s medicine
VI. Professional Insight: How Emotions Shape Patient Outcomes
Over time, I’ve come to realize that emotional healing doesn’t just influence recovery – it also shapes how patients interpret their care. Feelings of neglect, confusion, or dismissal can change how an experience is remembered, even when the medical treatment itself was excellent.
That’s why empathy, education, and communication matter just as much as medication and procedure. When patients feel supported, they don’t just recover physically – they learn to trust the process. And that trust becomes the quiet proof of compassionate care.
Every outcome has two stories – the clinical and the emotional. Healing happens when both are acknowledged
VII. Closing Reflection: Wholeness Beyond The Wound
A patient’s recovery is more than just watching a wound heal or recording vital signs. True recovery includes the emotional work that takes place beneath the surface – the part that requires patience, reassurance, and human connection.
Healing isn’t measured only by how quickly an incision closes, but by how gently the patient learns to trust their body again. The body heals through time, but the heart heals through connection. Every quiet “you’re doing great” and every moment of encouragement becomes a kind of medicine, stitching strength into the spirit long after the scar has formed.
Scars may close on the outside, but peace closes from within
Leave a comment